Kinematically Aligned Total Knee Replacement Surgery
A Personalised, Precision-Based SURGICAL Approach for Optimal Joint Function IN THE KNEE
Your knee is a highly complex joint that can be significantly impacted by arthritis, injury, or other conditions, leading to chronic pain and reduced mobility. For many patients, total knee replacement (total knee arthroplasty) offers a surgical solution to relieve this pain and restore function.
When you choose Dr Antony Liddell for your total knee replacement, your procedure is performed using advanced techniques, including the kinematic alignment (KA) surgical approach(calipered), which represents a more personalised and advanced proceduretechnique in knee replacement surgery. Unlike traditional surgery methods that use a one-size-fits-all approach, Dr Liddell customises the surgery to match your specific knee structure. This approach helps restore the natural movement of your knee, making it feel more like your own and potentially leading to better overall results.
In the following sections, we’ll take a closer look at kinematically aligned total knee replacement, explaining how personalised alignment works, the advanced technologies involved in this cutting-edge procedure, and what you can expect throughout your surgical journey.
WHAT IS KINEMATIC ALIGNMENT?
Kinematic alignment (KA) is a surgical approach that aims to restore the natural alignment of your knee by considering the unique angles, curves, and movements your knee had before arthritis or injury. This approach is important for both improving knee function and reducing the risk of complications that could affect other parts of your body after surgery. Misalignment during knee replacement can place extra strain on surrounding joints, such as the hips, spine, or opposite knee, potentially leading to further discomfort or issues over time.
By closely matching the new knee prosthesis to your natural joint structure, kinematic alignment helps maintain the body’s overall balance and biomechanics, which may help prevent problems that arise when other joints adjust to an unnatural knee alignment.
With kinematic alignment, the prosthetic components are positioned to replicate your knee’s original function, offering several potential benefits:
- Maintains natural joint alignment and movement: The prosthesis is carefully aligned to match the natural positioning of your bones, ligaments, and tendons, aiming to support the knee’s balance and movement.
- Restores natural knee biomechanics: This method seeks to replicate the original motion patterns of your knee, which may result in smoother, more fluid movements after surgery.
- Provides a more natural feel: Because the implant is aligned with your pre-arthritic knee structure, many patients report that their knee feels more comfortable and natural after the procedure.
- Calipered Kinematic Alignment is an extension of this technique, which focuses on enhancing precision during surgery. This advanced approach uses callipers and other specialised tools to measure and position the prosthetic components with a high degree of accuracy, aiming to closely replicate your knee’s natural dimensions.
During the procedure, Dr Liddell uses callipers to carefully measure the thickness of the bone and cartilage removed, ensuring that the prosthesis is closely aligned with your knee’s original anatomy. This added level of precision offers several potential benefits:
- Improved accuracy in implant placement: By using callipers, the prosthetic components are fitted with greater accuracy, which may help improve how your knee feels and functions after surgery.
- Potential for reduced risk of misalignment: Small misalignments during surgery can lead to discomfort or changes in movement. Calipered kinematic alignment aims to minimise this risk by ensuring that the prosthesis is placed in line with your individual knee structure, potentially offering greater stability and comfort.
- Enhanced longevity of the knee replacement: By positioning the prosthetic components more accurately, calipered kinematic alignment may reduce wear on the implant over time, which could help extend the life of your knee replacement and reduce the likelihood of needing revision surgery.
- Improved function and comfort: By closely replicating the natural structure of your knee, calipered kinematic alignment can support smoother movements and enhance comfort, potentially helping you return to daily activities with more confidence.
By opting for calipered kinematic alignment, you receive a personalised approach to total knee replacement surgery that focuses on optimising the function and comfort of your knee, potentially improving your quality of life after surgery.
THE KINEMATICALLY ALIGNED TOTAL KNEE REPLACEMENT SURGICAL STEPS
Kinematically aligned total knee replacement is designed to restore your knee’s natural movement and alignment by positioning the prosthetic components in a way that mirrors your original anatomy. This personalised approach is different from traditional methods, which often follow a one-size-fits-all alignment model. By focusing on your unique joint lines and bone structure, kinematic alignment may lead to a more natural-feeling knee and improved function after surgery.
Below is an overview of the key steps involved in the procedure, from pre-operative planning through to precise implant placement, using advanced instrumentation and surgical techniques tailored to your individual knee. Each step is performed with the goal of achieving optimal joint movement, comfort, and long-term durability.
The Surgical Process
A step-by-step guide to your surgery
1. Planning
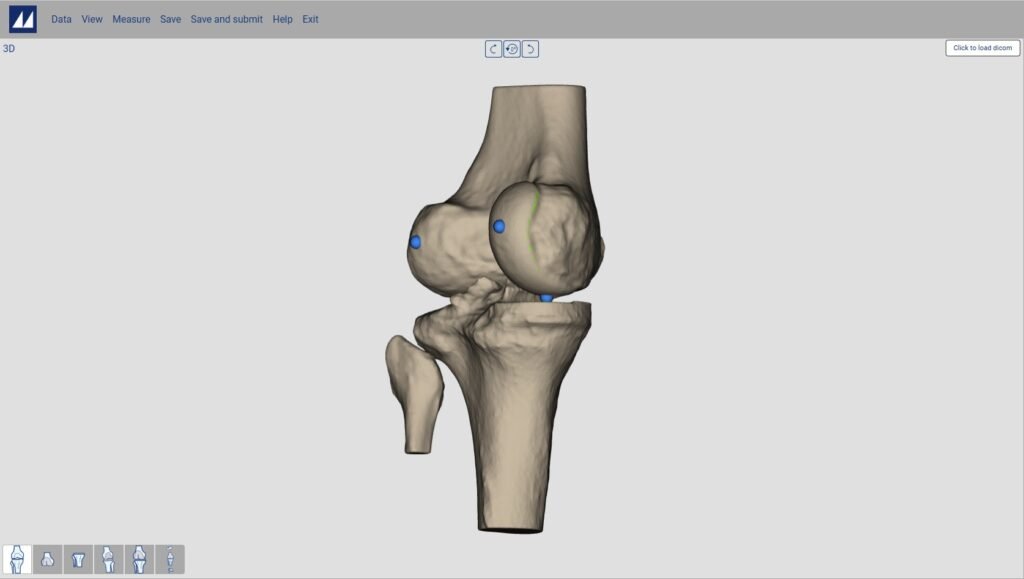
Using your CT Scans
Before surgery, Dr Liddell will use the detailed imaging, including your X-rays and a CT scan, to create a personalised map of your knee. These scans help identify the exact shape, alignment, and wear pattern of your joint. Using this information, Dr Liddell can plan your knee replacement procedure with a high level of precision. Every decision, from how much bone to remove to how the implant is positioned, is based on your individual anatomy. The goal is to restore your knee as closely as possible to how it moved and felt before arthritis developed.

2. Anaesthesia
Keeping you comfortable and safe during surgery
On the day of your procedure, you will meet with the anaesthetic team to discuss the most appropriate method to keep you comfortable throughout surgery. Options typically include either general anaesthesia (where you are fully asleep) or spinal anaesthesia (which numbs the lower half of your body while you remain relaxed and drowsy). The decision is based on your medical history, personal preference, and clinical factors. Once the anaesthetic is in effect, a tourniquet is gently applied around your upper thigh to limit blood flow to the area. This helps provide a clearer view of the joint during surgery and reduces bleeding. Your leg is then cleaned with an antiseptic solution and sterile drapes are placed around the surgical site to maintain a safe and sterile environment.
3. Surgical Access
Carefully opening the knee for accurate joint preparation
To begin the procedure, Dr Liddell will make an incision along the front of your knee to access the joint. The exact length of the incision depends on your knee’s anatomy and the complexity of the surgery. Throughout this step, Dr Liddell takes great care to minimise disruption to surrounding muscles and soft tissues, which can support a smoother and quicker recovery. Once the joint is exposed, any damaged bone, cartilage, or tissue is removed. Precision callipers are then used to measure the thickness of the removed bone. These measurements help ensure that the prosthetic components are matched accurately to your knee’s original structure for a natural fit and alignment.


4. Placement
Aligning the prosthetic components to match your natural knee
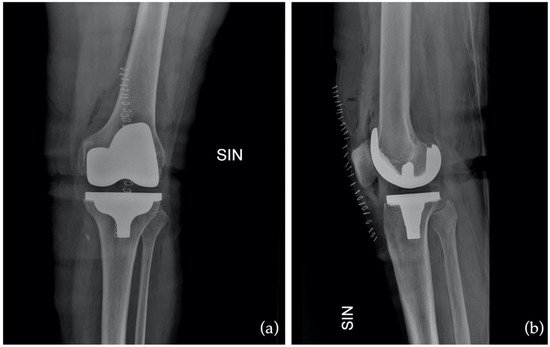
The key aim of kinematic alignment is to position the knee replacement components in a way that closely replicates the natural anatomy of your knee. Using precise measurements taken with callipers during surgery, Dr Liddell carefully places each prosthetic part to restore your original joint alignment and movement patterns. Femoral Component - A metal cap is placed over the end of your thigh bone (femur), replacing the damaged bone and cartilage. Tibial Component - A metal baseplate is secured to the top of your shin bone (tibia), and a polyethylene insert is added to act as a cushion, mimicking the role of natural cartilage. Patellar Component (if required) - In some cases, the underside of the kneecap (patella) is resurfaced with a smooth plastic layer to improve motion and reduce friction. This calipered kinematic alignment technique ensures that each component is positioned according to your individual anatomy. The goal is to create a knee that feels and functions as naturally as possible, potentially leading to greater stability, comfort, and long-term satisfaction.
5. Final Adjustments
Fine-tuning alignment, motion, and joint stability before closure
Once the prosthetic components are in place, Dr Liddell performs a series of final checks to ensure the new joint is properly aligned and functioning as intended. The knee’s range of motion, stability, and the fit of each component are assessed carefully. If needed, minor deformities such as bowlegs (varus) or knock knees (valgus) are corrected at this stage. The goal is to optimise the mechanical balance and movement of the knee to closely replicate your natural biomechanics. A surgical drain may be placed to help reduce fluid build-up within the joint after surgery, supporting a smoother recovery.

6. Closure
Protecting the surgical site and supporting early healing
Once the final adjustments are complete, the surgical site is closed with dissolvable sutures. The incision is carefully sealed to support healing while minimising scarring and risk of infection. A sterile dressing is applied over the knee to protect the area and promote a clean healing environment. The bandaging also provides gentle compression, helping to reduce swelling and support early post-operative recovery.
POST-OPERATIVE REHABILITATION GUIDELINES FOLLOWING A KINEMATICALLY ALIGNED TOTAL KNEE ARTHROPLASTY
Post-operative rehabilitation after a kinematically aligned total knee replacement surgery is a critical aspect of your recovery. It is designed to help restore knee function, improve mobility, and ensure the long-term success of your knee implant. Dr Antony Liddell and his team will work closely with you to develop a personalised rehabilitation plan that suits your individual needs and goals. Below is an overview of the key stages in your post-operative recovery and rehabilitation.
Immediately Post-Op
- Initial Recovery: In the immediate hours following your surgery, you will be taken to a recovery room where your vital signs, surgical site, and pain levels will be closely monitored. During this time, the medical team will ensure that pain management protocols are effective and that there are no early signs of complications such as excessive bleeding or infection..
- Early Movement: Depending on your condition and Dr Liddell’s assessment, you may be encouraged to begin moving your knee soon after surgery. This might involve assisted standing or walking with the help of crutches or a walker, typically within the first 24 hours post-op. Early movement is crucial in preventing blood clots and promoting circulation to the healing tissues.
Physiotherapy: Your rehabilitation starts in the hospital. A physiotherapist will guide you through gentle exercises aimed at improving knee mobility and preventing stiffness. These may include ankle pumps, quadriceps exercises, and knee bending while in bed. The goal is to regain a basic range of motion and ensure that you can begin weight-bearing activities as soon as your knee allows.
Pain Management: Effective pain management is crucial for early mobility. You will be prescribed a regimen of pain relief medications, which may include anti-inflammatory drugs or other medications. Proper pain control will make it easier for you to participate in rehabilitation exercises and accelerate your recovery.
First Few Weeks
- Home Exercises: Once discharged from the hospital, you will be given a set of home exercises designed to maintain and improve knee flexibility, strength, and range of motion. These exercises are critical for preventing stiffness and promoting long-term joint health. You will be encouraged to perform these exercises regularly to continue making progress.
- Ambulation Aids: Depending on your recovery progress, Dr Liddell may recommend continuing the use of crutches or a walker until your knee regains sufficient strength and balance. This is especially important to protect your knee while it continues to heal and ensure that you are moving safely.
Weeks 2-6
- Physiotherapy Sessions: During this phase, you will have regular physiotherapy sessions, where the exercises will become progressively more challenging. The focus will shift toward increasing your strength and improving your range of motion. Your therapist may introduce stationary cycling, heel slides, and strengthening exercises that target your quadriceps and hamstrings.
- Gradual Weight-Bearing: Based on your progress, Dr Liddell will advise on when to gradually increase the amount of weight you can put on your operated knee. It’s important to follow the prescribed weight-bearing restrictions closely to avoid putting unnecessary stress on the healing joint.
Weeks 6-12
- Advanced Strengthening: As your knee continues to heal, your rehabilitation will focus on more advanced strengthening exercises. This may include stationary biking, leg presses, and resistance exercises that target the muscles around your knee. The goal is to rebuild the strength and endurance of your leg muscles to support your new knee joint.
- Functional Activities: Your physiotherapy will also start to include functional movements such as walking up and down stairs, getting in and out of chairs, and other real-world activities that you’ll need for daily life. These exercises help restore confidence in using your knee for everyday tasks.
Beyond 12 Weeks
- Return to Normal Activities: By the 12-week mark, many patients are ready to resume a more normal routine. With Dr Liddell’s and your physiotherapist’s guidance, you’ll gradually return to low-impact activities such as recreational walking, swimming, and light sports. You will be encouraged to avoid high-impact activities like running or jumping, as these can put too much stress on the new joint.
Monitoring and Follow-Up Appointments: Regular follow-up appointments with Dr Liddell will continue throughout your recovery. These appointments are crucial for monitoring your progress, ensuring the knee replacement is functioning well, and addressing any concerns. Adjustments to your rehabilitation plan may be made as needed to optimise your recovery.
ADDITIONAL TIPS FOR A SUCCESSFUL RECOVERY
Recovering from total knee replacement surgery involves more than just rest, it requires active participation in your rehabilitation and daily care. In addition to following your physiotherapy plan and attending post-operative appointments, there are several simple but important steps you can take at home to support healing, reduce discomfort, and maximise the long-term success of your knee replacement including:
- Ice Therapy: Use ice packs regularly during the first few weeks to reduce swelling and discomfort. Apply ice for 20-minute intervals, ensuring a cloth or towel is placed between the ice and your skin to prevent frostbite.
- Wound Care: Keep the surgical site clean and dry. Dr Liddell will provide you with instructions for wound care and signs of infection to watch for, such as redness, warmth, or increased pain around the incision site.
- Adhere to Your Exercise Plan: Performing your prescribed exercises regularly is key to regaining function and mobility. Consistency is crucial in maintaining progress.
- Lifestyle Adjustments: Maintaining a healthy weight can reduce stress on your new knee, prolonging the life of your knee implant. You may also be advised to adopt low-impact activities like swimming or cycling as part of your long-term exercise routine.
These tips can help you stay on track and feel more confident during your recovery journey.